For many who overcome Covid, leaving the hospital is only the beginning of getting back to health. Eight Washingtonians recount the aftermath of beating the disease.
Diagnosed: May.
Days hospitalized: 5.
After a week of 102-degree fevers and visits to the doctor and ER, the nine-year-old from Fort Washington was diagnosed with Kawasaki disease at Children’s National. Kyree’s mother, Tammie Hairston, describes the aftermath.

“Kyree didn’t have the peeling of the skin, but he did have the pain and red eyes. He had gone through too many Motrins. Four bottles at the most. After they gave him medicine in his IV, he never ran another fever. We have followed up, since he’s been home, with the cardiologist. They think his heart skipped a beat. But it wasn’t anything severe. They wanted him to wear a 24-hour heart monitor. August was his last follow-up, and everything was clear. They said he can come off the baby aspirin—he had to take that once a day. Safety measures, because he had the inflammation of the valve. He’s gone back to his regular old self. It’s more me checking behind him every day. It’s the unknown that’s the fear. I’m one of those people that puts the macho hat on. When Children’s admitted him, I did break down and cry right there in the hospital because it was almost like a weight was lifted—it wasn’t an unknown anymore.”
Diagnosed: March.
Days hospitalized: 21.
The 60-year-old rector at Georgetown’s Christ Church was the first patient diagnosed in DC. He spent three weeks on oxygen at Georgetown University Hospital.

“For me, it was a steady recovery. My lungs had to clear, and that took over a month—I had a cough for two or three weeks. I lost 28 pounds, and all of that is muscle. I was very weak—climbing stairs left me tired. There was a period where I was a bit confused and found it hard to concentrate on things, but that seems to have gone away. My short-term memory was worse than it normally is. Writing a sermon initially took me much, much longer—probably 50 percent longer—and it’s harder to pull different items together. I had oxygen at home, but I hardly used it. I’m pretty much a hundred percent now, though I’m not as physically fit as I was. I went on a run the other day, and I can just about jog very slowly for a mile and a half, but before Covid, I could do twice that, easily.”
Diagnosed: April.
Days hospitalized: 7.
Eight months pregnant, the 34-year-old Frederick nurse tested positive after she stopped feeling her baby move. She was on oxygen at Adventist HealthCare Shady Grove Medical Center.

“The coughing went away two weeks after [discharge]. The taste came back a week or so after. A month or two later, my blood pressure was still elevated: 190-something and then 200, compared to now, 120s. Being a nurse, I’ll monitor myself, and usually if I feel lightheaded, I think my blood pressure is up. I’m like, okay, let me just lay down and drink water. [My daughter Kimora] was born May 8. Even after I had her, they had to give me three shots to bring my blood pressure down. The doctor was like, ‘Maybe it’s the labor effect.’ I was like, ‘I don’t think so!’ [She’s] healthy, and that brings joy to my heart. My other pregnancies, I didn’t have problems. With this one, there’s a little more fear and probably more attachment. I look at her and think: This is a corona baby.”
Diagnosed: March.
Days hospitalized: 52.
The 31-year-old project manager for a construction company, who moved to Northern Virginia from Colombia four years ago, spent five weeks on a ventilator at two Inova hospitals. He survived after a last-resort procedure: going on an ECMO machine, an apparatus that does the lungs’ work for them.

“I woke up. I forgot all the English I know—I forgot everything. They taught me how to walk, how to eat. I went to surgery on my lung—Covid caused pneumonia, and the pneumonia caused a blister inside my lung. The lung collapsed—it makes me cough. They told me, worst-case scenario, if the lung is not healing well, they need to take it out. I have back pain. Sometimes it’s so hard because I cannot find the correct position to sleep. I have bedsores. Sometimes [in the hospital] they flipped me over on my belly, so one of my arms got affected and I could not move it at all when I got home—I started [physical] therapy. Because of everything, the neurologist did some tests, and one showed I had a problem with my nerve. The neurologist said the nerve takes a long time to heal. I cannot be focused for too much time. I used to work on a computer for eight hours. Right now, I feel that I can be focused for two, three hours. My military training helped me a lot because in basic training it’s something like that: You are feeling that you cannot do it, but you make it.”
Diagnosed: April.
Days hospitalized: 10.
The 74-year-old from Brookeville was recovering from knee surgery when her physical therapist saw her struggling to breathe. An ambulance took her to MedStar Montgomery Medical Center in Olney.

“I couldn’t take a full breath. I felt like I didn’t have any appetite. I couldn’t taste anything. At the [ER], they told me I have water in my lungs. They took the test, and they said negative. At midnight, [the nurse] came to my room. She called the ICU. Then I went to the ICU, and it was positive. I was on oxygen.
“I got taste [back] in the hospital. I asked them for yogurt, and I could feel it tasted like yogurt. Now I can taste and smell better. [When I got home,] I stayed in one room for 14 days—I had to take it easy. It was hard, but I felt at home because when I was in the hospital, I felt I was by myself. I still can’t sleep very well thinking about it. I was thinking about my family, my friends, and my family in Greece—I have a brother and sisters there, so it’s hard. I feel back to normal, from before-coronavirus to after-coronavirus. The only thing I take now is what I used to take: my blood medicine and some vitamins.”
Diagnosed: March.
Days on a ventilator: 18.
The general manager at the Columbia Heights bar Red Derby, who is 51, got to Washington Hospital Center with a heart rate of 160 beats per minute. He was intubated once his test came back and was hospitalized for 38 days.

“The coma—I was shocked because I could hear so much. I heard this voice, and I’ve come to learn later that his name was [CNN host] Chris Cuomo. He said, ‘Yes, I have the coronavirus, but I will not let it define me,’ and then he said something along the lines of ‘I will not die like this.’ And that’s when I popped up and was like, ‘Me neither!’ That brought me out. One of the nurses was like, ‘We were all rooting for you because no one has ever come off a ventilator in our unit.’ I felt 25 when I went in, and I felt 75 when I left. I would take five or six steps and my heart rate would race up to 145. Every joint in my body hurt. That’s one of the lingering effects: My joints hurt every morning—up until [September 4], when I got a procedure done for atrial-flutter ablation. It’s supposed to regulate the heart rhythm. That was something directly related to Covid-19. I felt better on the way home [from the procedure]. When I got up in the morning, I was like, ‘I don’t feel winded.’ I have a stationary bike in the house, and I would get on that thing for five minutes. Now I can ride it for about 30 minutes and I feel great. I still have a few backaches and shoulder aches, just from being under for so long and in a bed for so long. My mobility is still limited. In the restaurant where I worked, there were three levels, so I was up and down stairs like 60, 70 times a day. Right now, I’m focusing on recovery, but ultimately the end goal is to get back in and working. It’s funny—now I feel my age.”
Diagnosed: Never, but symptomatic since March.
Days hospitalized: None, but considered a “long-hauler.”
The 39-year-old lawyer from AU Park was not officially diagnosed but has suffered symptoms and complications consistent with Covid since she was exposed. She belongs to a class of patients known as “long-haulers”: people who experience Covid effects for months.

“Before I got sick, I would run on average six miles a day. On March 21, I could barely walk. At the time, the understanding was not to go to the hospital, because if you don’t have it, you may get exposed. I didn’t get a test until 16 days after symptom onset. I was able to see a pulmonologist [on April 28]. My immunoglobulin level was slightly elevated—that indicates recent infection. Two days later, I’m on a walk, and I’m like, ‘I just need to lie down for a second.’ So I literally lie down in somebody’s yard. I see [the pulmonologist] again. He says, ‘You have a pericardial effusion—fluid around your heart.’ I started taking natural supplements, some Eastern medicine. All this time, I’m in bed. I could shower once every four days. It would be a big to-do. Eventually, I could sit outside. I would do a lap around our pool, just walking. I did that until I got to ten laps. Finally in late July, I could walk outside in our front yard. Still symptomatic, all the same things. I went to an orthopedic surgeon because my left median nerve was swollen. I couldn’t extend my left arm. I saw an ophthalmologist for head-pressure issues. I do physical therapy for respiratory health, I’ve done lymphatic-drainage massages. I have one of the best private medical-insurance plans you could have, but I’ve still probably spent around $20,000. I haven’t worked since March 20. I was like, ‘I have to piece this together. Otherwise, I’m never going to get the care I need.’ To have the weight of fighting for care while I’m literally feeling like death was tremendous. Completely unnerving, destabilizing, debilitating. My absolute worst nightmare. This is one of the traumas around it—I’m so afraid of everything.”
Diagnosed: April.
Days on a ventilator: 9.
The 37-year-old electrician and former Marine from Silver Spring spent more than two weeks at Adventist’s White Oak Medical Center.
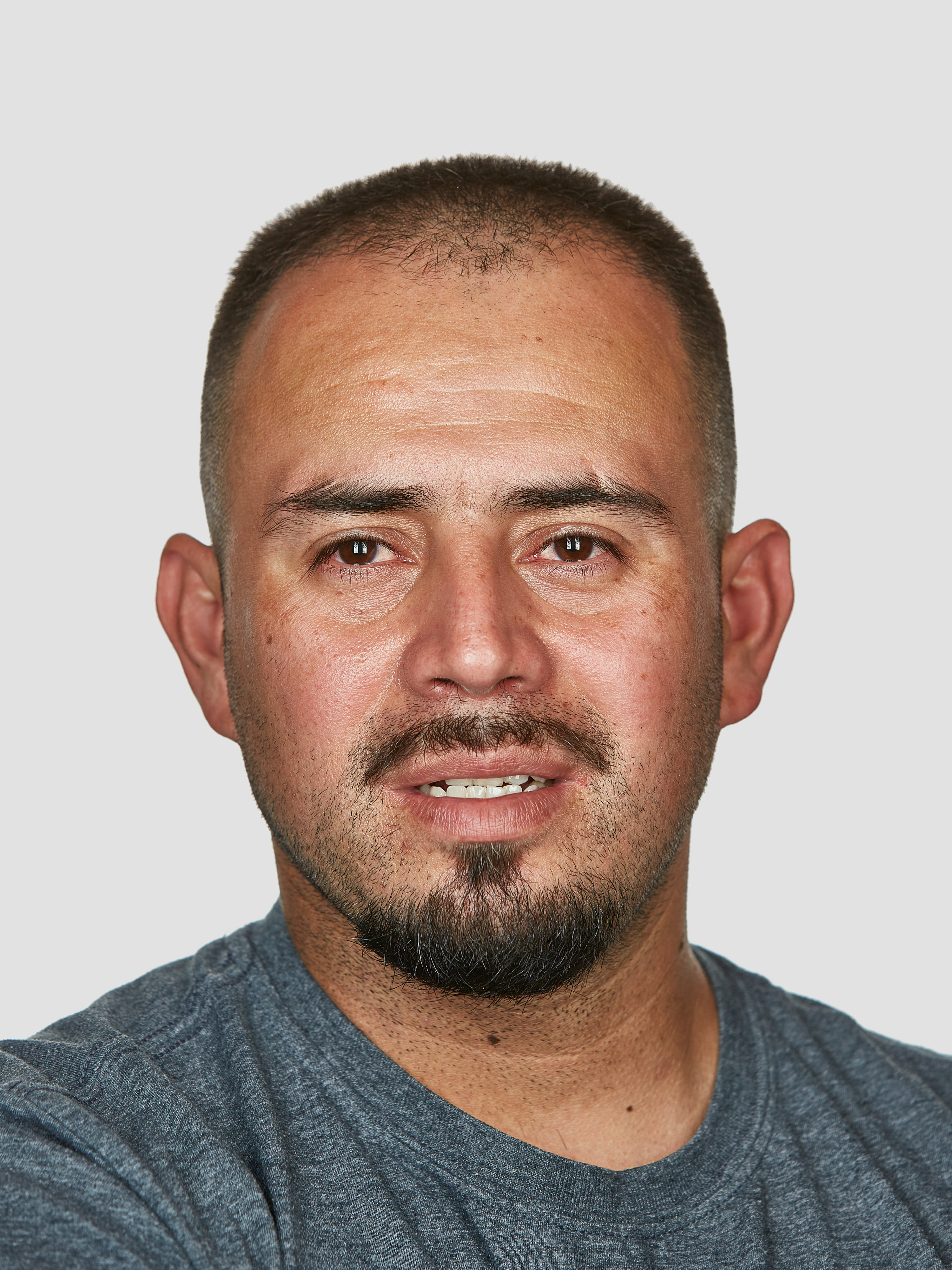
“I was skeptical of this virus. But when it got me, it got me really bad. My worst day was the day they took the machine off of me. I thought I was going to die. They stop the machine, but you’ve still got tubes up your throat. They leave you breathing by yourself. At first, they left me for an hour, then another hour. But then a third test, they left me for more than two hours. I didn’t think I was going to make it past a few minutes. I couldn’t find my remote for the alarm. I kept making noise. I had an IV line that I ended up ripping, so I was bleeding. The tube I was breathing on kept getting full with vomit because I vomited a few times. My left wrist was all purple because I was hitting the bed—my elbows were pretty bruised, too. I was almost giving up. The guy finally came and removed the ventilator. I felt like I was born again. For the first three days, [the nurse] had to pretty much pick me up out of bed. I couldn’t really talk much. I lost 30 pounds, and it took maybe three months to gain it back. After about a month at the house, I started working. The first week, it was rough. My legs were numb. Before, I was able to carry two bundles of conduit, and one day I couldn’t really carry one bundle. I had to call some of the young guys and say, ‘Carry this for me.’ I’d be coming from work and having a hard time getting from my car to my house, and there’s no steps. Just a straight shot. Now [six months later] I feel way better. I was running a lot before—a couple of miles. But I still haven’t tried it. I got chased last week by an eight-year-old for less than a minute, and I was out of breath. I had to sit down.”
This article appears in the November 2020 issue of Washingtonian.
"still" - Google News
November 16, 2020 at 07:00PM
https://ift.tt/335V2cD
8 Stories of People Who Recovered from Covid—and Still Deal With the Consequences - Washingtonian
"still" - Google News
https://ift.tt/35pEmfO
https://ift.tt/2YsogAP
Bagikan Berita Ini
















0 Response to "8 Stories of People Who Recovered from Covid—and Still Deal With the Consequences - Washingtonian"
Post a Comment