
Why are so many Americans still dying of COVID? The seven-day average is now 2,500 a day, higher than at any point in the last two years outside last January — before vaccines, at the height of the most devastating phase of the pandemic. Yesterday, the total reported dead was 3,600.
For those attuned to the ongoing, horrifying pandemic death toll, it may seem a continuation of the country’s failure stretching back to last spring. But more Americans died of COVID in 2021, the year Joe Biden took office armed with vaccines and promising a pandemic reboot, than in 2020, when Donald Trump bungled his way through everything but vaccine development. In the pandemic’s first year, defined by the campaign to “flatten the curve” and fights over mitigation measures like masks and school closures, the United States performed surprisingly poorly given its pre-pandemic reputation. But judging by COVID fatality rates, it was merely below average among the countries it considers its peers in the wealthy West, nearly all of which also struggled to enact the medical surveillance and cultivate the social trust necessary to curb spread without the help of vaccines. It was only in the pandemic’s second year, defined by the rollout of vaccines developed largely through American ingenuity and capital, that the U.S. has done far, far worse — by a large margin. “Since December 1, when health officials announced the first Omicron case in the United States, the share of Americans who have been killed by the coronavirus is at least 63 percent higher than in any of these other large, wealthy nations,” the New York Times calculated Tuesday. Compared to the countries with the lowest Omicron death tolls, the gap is much larger still.
The pattern predates Omicron. In early August, as the Delta wave was just beginning to accelerate, I wondered why so many more were dying here than in Europe; ultimately, the surge lasted through the fall, taking 200,000 American lives and producing the deadliest two-month period of the whole pandemic outside last winter. By early December, the American death toll was just as striking. And nearly as quickly as Omicron appeared here, there were signs that the United States would, again, depart from the European experience, where cases were exploding but with only a modest effect on severe outcomes and deaths. While the last few weeks haven’t fulfilled some worst-case scenarios, there are still 2,500 Americans dying every day now from a variant whose main advance billing was its mildness.
On Monday, the Financial Times published a staggeringly good, graphics-heavy digest of this phenomenon and some of the most likely explanations for it, namely low vaccine coverage and slow uptake of boosters. On Tuesday, I spoke with John Burn-Murdoch, whose work for the FT has made him one of the pandemic’s most trusted chroniclers and data gurus, about just how much more brutal the second year of the American pandemic has been and how much of that brutality can be explained by gaps in vaccine coverage of just a few percentage points.
Let’s start with the headline observation of your piece, which is just how much worse the U.S. experience has been. You suggest that if the U.S. was as well-vaccinated as most western European countries, only half as many Americans would’ve ended up in the hospital.
I first started to notice the gap with the Delta wave in July. As has too often been the case during the pandemic, the U.K. has often been at the front of some of these new variant trends. And we did see case numbers start to mount very quickly, but it became apparent relatively early on that hospitalizations and deaths were already a much smaller proportion of cases in the U.K. during the Delta wave than they had been during Alpha six months earlier.
Neither of the more acute indicators was getting anywhere near what they’d been in the previous winter, which was exactly what we’d been hoping we’d get with the vaccines. Whereas fairly early on in the U.S., we were starting to hear from places like Florida and elsewhere in the South and Midwest that the numbers were getting much closer to what previous waves had been — whether in the spring of 2020 or in the winter. And that just struck me.
Me too.
And when Omicron started taking off in the U.S., it again seemed to be doing something different to what we were seeing elsewhere — in western Europe and places like the U.K. We had seen a quite linear story as it was going from South Africa to the U.K. to the rest of western Europe, in terms of seeing these enormous records in case numbers, but with more acute indicators like hospitalizations not rising to as great an extent and not getting close to the previous peaks.
In the U.S., we haven’t gotten quite to the previous peak in terms of deaths, which came during the winter surge last year, entirely before vaccines. But we’ve passed that peak in terms of hospitalizations.
Now, I do think there are obviously some wrinkles here. Something that I think some people miss is if they look at a place like New York, and they say, Oh, hospitalizations have gone as high as they did last winter, they’re missing the fact that in a place like New York, the winter of 2021 was much less bad than the spring of 2020. But that being said, on the national level, we have seen hospitalizations and ICU admissions — and in parts of the U.S., deaths — get a lot closer to previous peaks than we are seeing in places like the U.K., western Europe.
Even in the country as a whole — if you take last January out of it, the seven-day average is now, at over 2,600, higher than it’s ever been. And though we probably won’t get as high as those January numbers, the average is still inching up. But before we focus on Omicron, I wanted to talk a bit more about Delta, particularly about the difference between its “presenting” severity, which also reflects the immunological context in which it emerged, and its inherent severity. Because everywhere in the world, the emphasis with Delta seemed to be on its enhanced transmissibility. But it appears also to have been clearly more severe. Without that playing a role, it would be impossible for a country like the U.S. — with more than half its population and three-quarters or more of its senior citizens vaccinated — to see its case-fatality ratio not budge from the pre-vaccine winter surge to the Delta wave.
I think this is such a fascinating thing. In the first couple of weeks of Delta, I was really quite surprised by how the narrative was forming around that. If we look at somewhere like the U.K. or many western European countries, because of very high rates of vaccination, Delta never presented on the population level as severe as Alpha. But there was never this conversation in May, June, or July of 2021 about things looking good with Delta, despite the fact that if one were to take a thousand cases of Delta and compare them to a thousand cases of Alpha, you would see less severe outcomes. Doctors were talking about this at the time, but it was always framed as a result of vaccination and other forms of immunity.
Which is not at all what’s happened with Omicron. I remember hearing from a lot of folks — doctors, scientists, epidemiologists — who were saying we didn’t need to resort to enhanced severity in our analysis of Delta, that the increased transmissibility alone could explain why we were seeing so many people in hospitals and dying.
All of these things were happening at the same time. But I think part of this is that it’s human nature that stories around things like this are formed not necessarily based purely on a rational, logical approach but just on a more emotional side. And I think the fact that India’s Delta wave was so bad, it led everyone to think of Delta as very, very bad, but then you saw it really well mitigated by the success of the vaccination campaign in the U.K. And so there was a sense of relief in places like the U.K. What started out being a very, very concerning few weeks at the end of May and coming into June — in the U.K., it fizzled out.
And I don’t mean that as in there weren’t deaths and hospitalizations, because there were. But looking at India, there were fears of something cataclysmic, and there were huge concerns about Delta’s ability to escape vaccine protection. And it turned out that, while there was some escape, it was relatively modest.
In your piece, you compare the severity of Omicron to Delta but not to Alpha or the original “wild-type” that emerged in Wuhan. What would that comparison be? My understanding is that Delta was more severe than the previous variants, which were more severe than the wild-type, and so even though Omicron is less severe than Delta, it’s in the neighborhood of the wild-type variant in terms of severity.
Yeah, that’s exactly it. My understanding is that Alpha was an increase in severity upon the wild type, Delta was certainly an increase in severity on Alpha, and Omicron — I’ve not seen exact numbers comparing it to the wild type, but I believe it’s in the same ballpark.
With Omicron, some of the best research on the specific question of intrinsic severity was the stuff done by Imperial College. Their best effort gets you to a reduction of intrinsic severity somewhere in the region of 30 to 50 percent.
Compared to Delta, you mean.
Yes. I personally have been using a very rough approximation of roughly half as severe because some other studies — which, to be fair, didn’t do as much work as Imperial College in terms of controlling for prior infection — were often finding somewhere between a half and two-thirds reduction.
There was also a study from South Africa recently where they found a smaller reduction in inherent severity — just 25 percent, I believe, which is quite striking given how much less severe it looked than their previous wave if you didn’t correct for how much more immunity had been gained since the last wave.
One additional thing I think really got lost in the noise in the early days of discussions about Omicron was not just the question of immunological context but Omicron’s immune escape.
One recent report found that more than two-thirds of British Omicron cases have been reinfections. And the same dynamic probably explains why the early spread in many countries was among the vaccinated.
If you take a thousand Omicron cases and a thousand Delta cases, the Omnicon cases will just be more heavily skewed toward people with some immune protection. And therefore, even if there were no change in its intrinsic severity, that would still mean it would look less severe.
But a lot of this stuff has gotten blurred, which is what we were trying to get at in our piece: The general reduction in the severity of COVID over the last two years has not just been some kind of natural blanket change that has happened in the same way everywhere. And it seems to be the case that countries that have patchier vaccination coverage, especially in their elderly and most vulnerable groups, have just not seen that same reduction in realized severity.
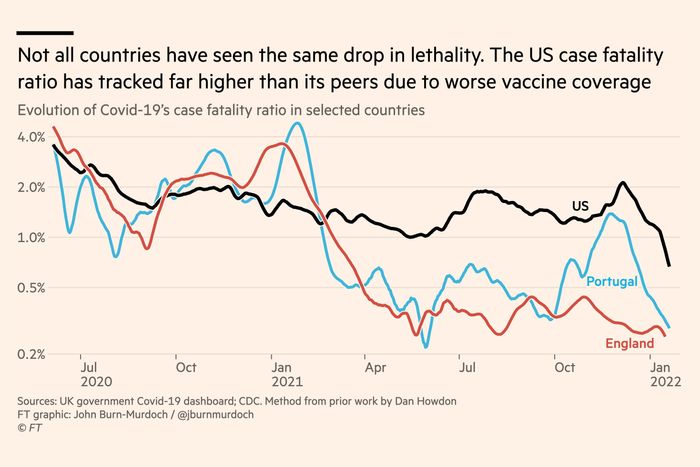
Which is worrying to consider when you think about parts of the world where vaccination rates may be low or very low and exposure to previous waves may also be pretty low. But in certain ways what’s most striking about that data is the American experience, which is to say the American anomaly. Personally, I just can’t get over the fact that for the U.S., 2021 was worse than 2020 — in terms of the total number of deaths but also in terms of our relative performance compared to our peers, who all saw pretty dramatic reductions in fatality rates. In the U.S., before Omicron, our case-fatality rate hadn’t declined at all, as one of your charts illustrates powerfully.
Part of that story is about the exact timing of the calendar year. With Alpha, the U.K. saw a lot of bad outcomes — hospitalizations and deaths — at the back end of 2020. That makes the U.K.’s 2020 look particularly bad and 2021 slightly less bad.
But the U.S. did certainly start vaccinating ahead of pretty much every other country in the world other than Israel.
And yet by the time Delta rolled around, we had fallen behind almost everyone.
With the Delta wave in the U.S., you had this perfect storm. Number one, relatively low vaccination rates in places like Florida–
Really low vaccination nationwide. There are problems with our data, which might be most noticeable in Florida, but at least the official vaccination rate in that state is about average for the U.S., not below. Which is one reason it was so striking, even given the large number of elderly people that live there, that Florida had by far the worst Delta surge of any state in the whole country. It doesn’t seem to make sense, which is one reason to be additionally skeptical of those vaccination figures.
Yes. On that point, we did a story earlier in the year about the quality of vaccination data out of parts of the U.S., with Florida being the prime example. There were numbers purporting to say that Florida’s vaccination coverage among elderly groups is very, very, very high when a large number of the people who have been counted as vaccinated seniors in Florida were actually people who had come from other states to Florida, got vaccinated, and then left.
In certain zip codes, they didn’t just report vaccination coverage above 100 percent, they reported coverage about 200 percent.
And I think what that means is that what looked like smaller gaps in vaccine coverage among the vulnerable between the U.S. and the U.K. ended up being bigger heading into the Delta wave, certainly in parts of the U.S.
To get back to the U.S. fatality anomaly, you mentioned vaccination coverage …
And then the southern states were also those that had been hit less hard the previous spring. And so these were places that had both less immunity acquired by vaccination and less immunity acquired by infection. Whereas in Europe, most places had pretty good vaccination levels and had been through very, very steep winter waves just in the previous winter. I mean, if we look at deaths over last winter, for example, it is not just the U.K. but countries like Portugal as well that had extremely bad waves then.
There are other factors that contribute as well. One thing that gets mentioned a lot is the relatively high levels of obesity in the U.S.
But just to cut you off — obesity is obviously a risk factor, but looking at the data, none of these comorbidities come close to the effect of age. Even the worst of them — transplant patients, immunodeficiencies — are only the equivalent of adding 10 or 15 years to your age. Most of them, including obesity, have a much smaller effect.
Yes. That’s right.
So how do you explain the huge gap in outcomes? We hear an awful lot about vaccination coverage, and it was the focus of your piece, but the numbers aren’t all that different. In the U.K., I believe, 77 percent of the population as a whole has gotten at least one shot and 71 percent has been double vaccinated. In the U.S., the numbers are 75 percent and 64 percent. That’s a gap, of course, but it isn’t enormous. And where it really matters, among the vulnerable elderly, the gap is smaller. In the U.K., 95 percent of those over 65 have gotten one shot, and 93 percent have been double-vaccinated. In the U.S., officially at least, the numbers are 95 percent and 88 percent. There is a difference there, but is it sufficient to explain the dramatic divergence in case-fatality rate between the two countries? For most of this year, the U.K.’s CFR has been two to three times lower than ours — and at a few points, it’s been as much as six times lower. That means for any given number of cases, about one-third as many Americans have died as Brits. Can a 5 percent gap in the coverage of the elderly really explain that?
I think something that’s really important to the discussion here is that it has not been ideal that we have always talked about vaccine effectiveness by talking about these numbers out of 100 percent. You say something is 90 percent effective or 80 percent effective when talking about the vaccines themselves, and similarly, when you talk about vaccination coverage, you say you’ve got 90 percent of people vaccinated or 80 percent. But the important figure is actually the inverse of that — it’s the hundred minus that.
Because a place that’s got 90 percent coverage and a place that has 85 percent coverage — those numbers sound similar, but actually one has 50 percent more vulnerable people, which is a huge gap.
Exactly that. And that explains some of the head-scratching that we’ve all been doing over the last couple of weeks looking at the U.S. versus the U.K. and western Europe. People will say, Well, look, the U.S. has got around 95 percent of its seniors protected — perhaps even more than 95 percent of its seniors vaccinated with two doses now.
Putting aside the subject of boosters for now …
Yes, without even getting into things like that, the US could have 98 percent double vaccinated and western European countries could have 99 percent double vaccinated.
Which sounds like no difference.
But it is a 100 percent difference.
Doesn’t that mean capping vaccination rates at any level could be misleading? If your cap is 95, like the CDC’s, and one place is at 96 and another is at 99, that difference is really quite large.
Right. For that reason, I actually capped it at 99, partly because some countries that do have really good data are showing uptake as high as that among the elderly.
Although built into that is the assumption that a country that is reporting a higher than 99 percent uptake does in fact have at least 99 percent coverage, right?
Absolutely, absolutely. And I’d be the first to say, in terms of the analysis that we did, that’s the biggest limitation with the data that we used. One percent versus 2 percent is a huge difference. It could also just be an error. It could also be a rounding error. There could actually be no difference. So these things are very sensitive to measurement
But even using the measurements we do have — looking at the difference between the U.K. and the U.S., it’s the difference between 29 percent of one country being unvaccinated and 36 percent of the other country being unvaccinated. That’s not even a 100 percent difference, let alone a 200 percent or 300 percent or 600 percent difference — it’s a 25 percent difference. And zooming in just to the elderly, it’s the difference between 7 percent of the elderly being vulnerable in one country and 12 percent in the other — which still isn’t a 100 percent difference. It’s a 70 percent difference. And for most of the fall, the U.K. case-fatality rate was three times as high. For a stretch there, it was six times as high.
You’re talking about the Delta wave in particular?
Yeah. We can talk about Omicron in a bit.
Well, I think there are a few things there. One is prior immunity. This is not something we built into our analysis the other day because it’s much harder to get very precise estimates for that. But the U.K. had a very, very, very bad winter wave at the end of 2020 with a very, very large number of infections, which meant that when Delta hit both countries, a significantly larger percentage of the population in the U.K. had been impacted previously than in the U.S.
In general, I think infection-acquired immunity has been something that’s been underdiscussed throughout the pandemic. It’s almost been this taboo to suggest that there may be other ways to reduce one’s vulnerability to severe disease in addition to getting vaccinated because no one wants to encourage people to go out and get infected. But those people who have been infected do have protection.
I sent you some data from New York State, where the gap in vaccination coverage is even smaller compared to the U.K. The U.K. has 71 percent of its overall population double vaccinated, including 93 percent of those over 65. In New York, the numbers are 73 percent and 90 percent. These are very similar numbers — even working backward from 100 percent, you have only 40 percent more vulnerable elderly people in New York. And yet there is still this twofold or threefold difference between how many people are dying in New York compared to how many are dying in the U.K. Is that a function of infection-acquired immunity? That the major New York exposure was now so long ago — in the spring of 2020 — that there’s been significant waning, whereas the exposure in the U.K. has been more recent, suggesting less waning?
Yeah. But look, all I’m doing here is saying things that to me could reasonably explain the data you sent. And I do think that some of this comes to prior immunity. New York had one really bad outbreak, in spring 2020. The U.K., consistently from April 2020 until November 2021, was probably having more severe disease than New York. Second, boosters could be playing a role there.
Right. But before we get to boosters, is testing playing an important role here? If one country tests a lot more than another, it’s likely to pick up more mild cases, which would drive its case-fatality ratios down.
I think it certainly could play a role. But from what I’ve looked at in the U.K., the trajectory of case-fatality ratio is a very, very, very close match for the trajectory of the infection-fatality ratio.
Another thing to keep in mind is our analysis was primarily about hospitalization rather than death. If we’re talking about deaths rather than hospitalizations, the age gradient is ever steeper, which means that similar magnitudes of difference in immunity levels can manifest in even steeper differences in mortality rates.
And if a 95-year-old is 15 times more likely to die than a 65-year-old and hundreds of times more likely to die than a young adult, small variations in the demographic mix or in the vaccination coverage among the very old can make a very big difference overall.
Right, and if we look at the height of the waves, during Delta, as you say, the U.S. was significantly higher at the peak of its Delta wave. But I’m seeing more like a threefold increase in the height of daily death. And the data I’ve been looking at on vaccination coverage shows that about 90-odd percent of over 65 in England had been double vaccinated by that stage, whereas in the U.S., it was around 75 percent. So that gets you into that region of two and a half or three times the exposure, which to me seems broadly consistent with the magnitude of difference in deaths we saw at that time.
But let’s toggle over to your case-fatality data. I see the CFR in England, at the peak of its Delta surge, is well below 0.5 percent — probably about 0.3 percent or 0.35 percent. In the U.S., at the peak of our Delta surge, we’re pretty close to 2 percent. Depending on exactly how you want to make the comparison, it looks like more than a threefold increase to me — you could make the argument that it’s more like fivefold, maybe even a little more.
But interestingly, the gap is largest in early December, just before Omicron, as the lingering Delta wave started a second surge. There, the U.S. CFR reaches a new peak above 2.0 percent, which means that, as a percentage of total recorded cases, more Americans were dying of COVID than during the last winter surge, which took place entirely before vaccination. This peak was in early December, with more than 70 percent of the country vaccinated, including more than 85 percent of seniors and, by some estimates, more than 85 percent of the country already exposed to COVID in some form or another. In England, by contrast, the CFR at that point was 0.3 percent or so — about seven times lower.
That’s where prior infection and boosters were doing a lot of work in England. England had this slow-burning Delta wave in which a lot of people were getting infected, particularly younger people, and that was just adding a huge amount of immunity. And then the English booster rollout was pretty rapid once it got going — pretty fast and pretty steep. So I think the magnitude of that difference that we see in early December is really the result of those two factors — infection-acquired and booster-acquired immunity. But the gap during the Delta wave is roughly in this two- to threefold, maybe threefold ballpark.
The thing that’s most striking to me about this chart is not necessarily the divergence between the countries, it’s how flat the American CFR remains all year despite mass vaccination. It doesn’t fall much, even though more than 200 million Americans have been vaccinated, including the large majority of the elderly.
You could say it roughly halves from October 2020 to pre-Delta spring and early summer.
Right.
But again, that’s a halving that looks very small compared to a much, much bigger decline in western Europe.
It’s just so striking to me — 200 million doses of very effective vaccines managed only to fight Delta to a draw.
The really important thing for me here is the dosing interval.
That’s the length of time between the first and second dose.
The U.S. followed a three-week dosing interval. The U.K. was between an 8- and 12-week interval. Canada also went for the longer interval. European countries were somewhere between the two. A lot of them started doing four and then ended up widening the gap.
Do you think that made a big difference?
In one of the U.K. health security agency studies, there was around a twofold drop in vaccine effectiveness for a shorter dosing interval.
And then there was a study that came out relatively soon after that looking at two-dose efficacy against Delta in Canada and in the U.S. And that also seemed to be showing much faster waning of efficacy in the U.S. than Canada, with dosing interval one of the likely keys there.
So I think that’s something that’s probably still been underdiscussed because, for a long time, we didn’t know which of those dosing intervals was going to be the best. I think anyone who says they knew the longer interval was always going to be the better one — I think that’s a bit of hindsight bias. There were qualitative reasons to believe that a longer interval may be better, but I don’t think we can say England just completely nailed the science on that one. I think it was probably a bit of luck. But that would certainly explain why you would see a more modest payoff essentially for the same number of vaccines in the U.S. than you would elsewhere.
Right. Just to take that number seriously — a twofold reduction. That means that two-dose vaccine efficacy in England could be the equivalent of two-dose-plus-booster efficacy in the U.S. It’s like we’re starting out one shot behind, and we had to get the booster even to get to where the U.K. was pre-booster.
If you look at that CFR chart, again, all the countries started around 2 percent going into winter 2021. And then the U.S. comes down to one percent, and the others come down below 0.5 percent. And if we say, very roughly, that that shorter dosing interval had a twofold impact, then the U.S. could have been down at that 0.5 percent line, which is much closer to Portugal.
It probably means we’re a little higher than Portugal but the same ballpark.
Yeah. Now, I don’t have definitive proof or anything approaching that saying that that was the factor, but I think based on what we know, some of that difference, and perhaps a significant amount of that difference, could be explained by the dosing.
Let’s talk a bit more about boosters. The headline of this piece was “Pandemic of the Unboosted,” and I think there’s a growing view among American epidemiologists that part of the story of America’s poor performance is that while we may be relatively close in terms of overall vaccine coverage and probably a little farther in terms of our elderly coverage with two doses, the gaps are really, really large at the moment in the booster uptake. Between the U.S. and many European countries, there’s a 20-point gap, in some cases higher, and often higher when just looking at boosters among the elderly.
When I hear that analysis, it seems absolutely right in theory. But when I look at the CDC data, I see a relatively small share of deaths now among the vaccinated, which is a group that includes the double-dosed but unboosted. All told, all vaccinated deaths account for only about a fifth of recent deaths in the latest quasi-national CDC update. That ratio is about the same as it was during Delta, before waning was really a pronounced problem and before anyone had really begun booster rollout. So how large a role could boosters be playing in this divergence now if no greater share of deaths is among the vaccinated than before?
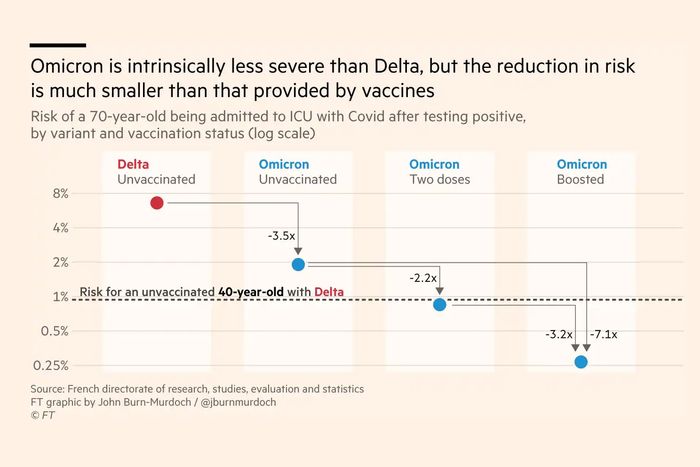
Yes, this is a really interesting one. Before doing this piece, I thought we would see a bigger difference between unvaccinated and double-vaccinated than we’d see between double-vaccinated and boosted. But once we look at the actual vaccine efficacy data, it does seem that those impacts are actually closer to one another in terms of the scale of protection.
In your piece, you estimate that two-dose vaccination reduces risk with Omicron 2.2-fold, and the effect of adding a booster is even bigger, more than threefold compared to two doses and more than sevenfold compared to the unvaccinated.
But I do think there’s also an important caveat there looking at the risk of hospitalization. We don’t have very good estimates yet for protection against death with Omicron. And it may be that the difference between two and three doses when it comes to death is smaller than the difference between zero and two doses. Whereas for hospitalization, the two differences might be similar.
And on hospitalizations, I think part of this story is health-care capacity. You’ve got to factor in the fact that the U.S. has a larger health-care capacity. This is an overarching point for the whole discussion: The U.S. has more health-care capacity than a place like the U.K. And therefore is perhaps able to admit patients with slightly less severe COVID than we’re seeing in the U.K.
But to pause there for a second, it raises a bigger issue, which relates to the question of boosters as well. In theory, it doesn’t make sense that this data would look different at the individual level and at the collective national level because — again, in theory — all that is happening as you’re just multiplying the individual risk factors by however many people there are.
But it is also the case that there has been this apparent gap, which we’ve been talking through in various ways already. We know that vaccines work very well, and we know that those people who have been vaccinated are very safe. We also know the majority of Americans and the large majority of seniors are vaccinated. And yet, we are still seeing some quite striking death totals and a case-fatality rate that, before Omicron, had not fallen at all from the bleakest period of the pandemic, which was entirely before vaccines. So we do have a different picture when we look at the national level than we might expect, looking at the vaccine efficacy data. And with boosters, the same curious gap applies: Given what we know about how few Americans have gotten them and about how much two-dose immunity wanes, especially among the elderly, I would expect to be seeing, during Omicron, a growing share of deaths among the vaccinated but unboosted. But that doesn’t seem to be what we are seeing. Instead, the Omicron surge in the U.S. is dominated by deaths among the unvaccinated, which suggests — to me, at least — that the large gap between U.K. Omicron severity and U.S. Omicron severity can’t be reducible to booster effects.
Yeah. I think some of the issue may be with the difference between hospitalization and death data for Omicron. The reason we used hospitalizations rather than death for this story is that we don’t have as good estimates of vaccine efficacy against death yet. And I think it’s entirely possible that just as protection against hospitalization with Omicron has eroded by less than the protection against infection has, it may also be that the protection against death has eroded by even less than protection against hospitalization.
Which would mean that while hospitalization figures may reflect a big booster gap, there is a smaller effect on death numbers.
There are definitely still moving parts here, and I think all our analysis can say is that for hospitalizations, it looks like the difference between two and three doses has a similar impact as the difference between zero and two doses. But when it comes to death, that may not be the case.
Last question. Looking at that same chart we keep coming back to — the one comparing the case-fatality ratio of the U.S. and Portugal and England. One notable feature is just how dramatically the CFR is dropping right now in the U.S. And maybe even more so in Portugal. What is going on here? Are we “catching up” to other countries in terms of immune protection? And if so, what would explain that — given that our vaccination numbers are pretty flat and our booster rollout has basically stalled?
Perhaps our bigger Delta wave has contributed some protection through natural exposure, but while it was significant, it doesn’t seem plausible to me that there was a major increase in infection-derived immunity between October and December — does it to you? You mentioned the Imperial College estimate and your rule of thumb that Omicron represented a reduction of severity between 25 percent and 50 percent. Looking at this chart, that is something like what we’re seeing in England. But in the U.S., the decline with Omicron has been much more pronounced — from above 2 percent to about 0.75 percent. Why is that drop so large?
In Portugal, I think what we’re seeing there is the transition from Delta to Omicron plus boosters. Portugal’s booster campaign was relatively late.
Which is one reason why they have such a high peak in the late fall.
Yeah, exactly. That’s Portugal.
In the U.S., it’s harder to say. The U.S. is doing a bit more boosting — some people will have encountered Omicron on the news and thought, Well, this is more reason to get a booster. Whereas in England, England’s booster push came pretty much entirely before Omicron arrived. I think that’s part of why the U.S. drops are slightly steeper. But beyond that, I don’t know, to be honest.
Sometimes — probably less often than I should — I look at some of these charts and I think, I don’t know entirely what’s happening there.
It does seem pretty mysterious, though also — possibly — encouraging. In early January, using that 25 percent reduction figure, I wrote that it was possible the country could hit 5,000 deaths a day and maybe even more. But that no longer seems possible, mercifully.
What’s going to be really interesting is if we come back to that CFR chart in a month — has the U.S. line come all the way down to join Portugal and England? Or has it seen that threefold drop and then found a new plateau? I think that would tell us how much of this was due to boosters and how much of it was due to other factors. But in the meantime, I don’t have a nice, neat explanation for exactly what we’re seeing in that one.
"still" - Google News
February 03, 2022 at 07:00PM
https://ift.tt/gUMZtxQEy
Why Are So Many Americans Still Dying of COVID? - New York Magazine
"still" - Google News
https://ift.tt/FP41nBZUm
https://ift.tt/7jqUa0fJp
Bagikan Berita Ini














0 Response to "Why Are So Many Americans Still Dying of COVID? - New York Magazine"
Post a Comment